Calm Logic
GLP-1 Specialist
My internist told me yesterday to raise my dose of tirz to 15 mg since that will help with my concern about low TST levels (since greater weight loss will help raise TST more).
Regarding lab values for testosterone in obese men:
Elaboration by Google Gemini:
Regarding lab values for testosterone in obese men:
Also most obese folks have low total testosterone. So every research study will have a low total testosterone patient if obese. A total testosterone means nothing in an obese patient . A free/ bioavailable is better. Low total testosterone in the obese doesn’t mean they need replacement.
Elaboration by Google Gemini:
Let's break down why total testosterone can be misleading in this population and why free or bioavailable testosterone is often a better indicator.
Why Total Testosterone is Misleading in Obese Individuals
- Increased Sex Hormone-Binding Globulin (SHBG):
- Obesity, particularly visceral obesity (fat around the organs), is associated with lower levels of SHBG.
- SHBG is a protein produced by the liver that binds to sex hormones, including testosterone, estrogen, and DHT. When testosterone is bound to SHBG, it's largely inactive and unavailable to tissues.
- Counterintuitively, while you might expect lower SHBG to mean more free testosterone, the overall hormonal milieu in obesity often leads to a complex interplay.
- Increased Aromatase Activity:
- Adipose tissue (fat cells) contains an enzyme called aromatase.
- Aromatase converts androgens (like testosterone) into estrogens (like estradiol).
- In obese individuals, especially those with a large amount of adipose tissue, there's increased aromatase activity. This means more testosterone is being converted into estrogen, leading to lower total testosterone levels and potentially higher estrogen levels. Higher estrogen can also feedback to the brain and further suppress testosterone production.
- Insulin Resistance and Inflammation:
- Obesity is often accompanied by insulin resistance and chronic low-grade inflammation.
- These factors can directly impact the hypothalamic-pituitary-gonadal (HPG) axis, which regulates testosterone production. Insulin resistance can impair Leydig cell function in the testes, and inflammation can suppress GnRH (gonadotropin-releasing hormone) and LH (luteinizing hormone) secretion from the brain, leading to reduced testosterone synthesis.
Why Free/Bioavailable Testosterone is Better
Given the factors above, here's why free and bioavailable testosterone provide a more accurate picture:
By measuring free or bioavailable testosterone, clinicians can get a better sense of how much testosterone is actually available to the body's tissues, regardless of the total amount or SHBG levels.
- Free Testosterone: This is the portion of testosterone that is not bound to SHBG or albumin. It's the biologically active form that can readily enter cells and exert its effects.
- Bioavailable Testosterone: This includes free testosterone plus testosterone loosely bound to albumin. Testosterone bound to albumin can also dissociate and become available to tissues. Testosterone bound tightly to SHBG is generally not considered bioavailable.
Why Low Total Testosterone in Obese Individuals Doesn't Automatically Mean They Need Replacement
This is the crucial point you've made. Here's why:
- The Root Cause is Often Obesity Itself:
- The low total testosterone in obese individuals is often a consequence of their obesity (increased aromatase, altered SHBG, insulin resistance, inflammation).
- Simply giving exogenous testosterone without addressing the underlying obesity is like treating a symptom without addressing the disease.
- Benefits of Weight Loss:
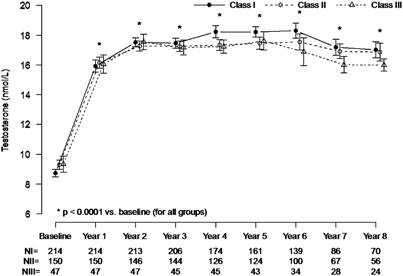
- Numerous studies have shown that significant weight loss (through lifestyle changes, bariatric surgery, or medication) can lead to a substantial increase in endogenous testosterone levels in obese men.
- Weight loss reduces adipose tissue (less aromatase), improves insulin sensitivity, and decreases inflammation, all of which can restore normal HPG axis function.
- Potential Risks of Unnecessary Testosterone Replacement:
- Giving testosterone to someone whose low levels are primarily due to obesity can suppress their natural testosterone production even further.
- Long-term testosterone replacement carries its own risks, including cardiovascular issues (though this is debated and complex), erythrocytosis (increased red blood cell count), prostate issues, and suppression of fertility.
Clinical Implications
- Comprehensive Evaluation: When an obese patient presents with symptoms of hypogonadism (fatigue, low libido, erectile dysfunction, depression, etc.) and low total testosterone, a clinician should always measure free or bioavailable testosterone.
- Focus on Lifestyle Intervention: The primary recommendation for obese individuals with low testosterone should almost always be aggressive weight loss and lifestyle modification. This addresses the root cause and often resolves the testosterone deficiency naturally.
- Careful Consideration for Replacement: Testosterone replacement therapy might be considered in obese individuals only after a thorough evaluation, including confirmation of consistently low free/bioavailable testosterone, a comprehensive discussion of risks and benefits, and often after attempts at weight loss have been insufficient to normalize levels or alleviate symptoms.
Last edited: