moonpies4misfits
GLP-1 Specialist
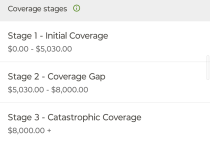
I'm so mad right now. I had a doctors visit back in August that my insurance is refusing to cover. It was a standard follow-up with my PCP where we also happened to also talk about weight loss options. No treatment, no prescriptions, we just discussed possible options.
Well, as it turns out, simply getting diagnosed with obesity means my visit is not covered. The exact wording I was given was "the claim was billed with a diagnosis that is specifically excluded from the plan." I am freaking livid. I pay for the highest tier of insurance my company offers. I'm paying extra money for "better" coverage but I'm not allowed to simply talk about being fat with my doctor without having to pay out of pocket?
Needless to say, I will be asking my doctors office to rebill the insurance company.
Edit to add: These are the codes that my insurance company referenced when they said my visit was not covered.
ETA 2.0: Confirmed that the CPT code is one that has been used before without issue, so this really is falling all on the obesity code being used.
Well, as it turns out, simply getting diagnosed with obesity means my visit is not covered. The exact wording I was given was "the claim was billed with a diagnosis that is specifically excluded from the plan." I am freaking livid. I pay for the highest tier of insurance my company offers. I'm paying extra money for "better" coverage but I'm not allowed to simply talk about being fat with my doctor without having to pay out of pocket?
Needless to say, I will be asking my doctors office to rebill the insurance company.
Edit to add: These are the codes that my insurance company referenced when they said my visit was not covered.
- 99214: Established patient office or other outpatient visit, 30-39 minutes.
- E66.9 Obesity, unspecified
ETA 2.0: Confirmed that the CPT code is one that has been used before without issue, so this really is falling all on the obesity code being used.
Last edited: