BioDad
GLP-1 Apprentice
I'm not sure if this study was posted here yet, but the long and short of it is...
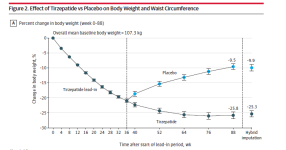
Obese adults did 36 weeks of tirzepatide + lifestyle modification (500 kcal/day deficit + ≥150 min/wk activity). After 36 weeks, the group was randomized and split into a tirzepatide group and a placebo group, which is just evil, for 52 weeks.
Despite remaining on the lifestyle interventions, in the placebo group, 82.5% regained ≥25% of the weight they had lost within 1 year, and cardiometabolic improvements (waist, BP, glycemic markers, lipids/insulin resistance) reversed in proportion to the amount of weight regained.
Worth a read and at the very least, a peek at the graphs - the 36 week divergence in weight is significant.
Obese adults did 36 weeks of tirzepatide + lifestyle modification (500 kcal/day deficit + ≥150 min/wk activity). After 36 weeks, the group was randomized and split into a tirzepatide group and a placebo group, which is just evil, for 52 weeks.
Despite remaining on the lifestyle interventions, in the placebo group, 82.5% regained ≥25% of the weight they had lost within 1 year, and cardiometabolic improvements (waist, BP, glycemic markers, lipids/insulin resistance) reversed in proportion to the amount of weight regained.
Worth a read and at the very least, a peek at the graphs - the 36 week divergence in weight is significant.